Content on this webpage is provided for historical information about the NIH Clinical Center. Content is not updated after the listed publication date and may include information about programs or activities that have since been discontinued.
"The safety of our patients and staff cannot be jeopardized." — Dr. Jim Gilman, CEO Clinical Center
COVID-19 is an emerging, rapidly evolving situation. Get the latest public health information from CDC. Get the latest research information from NIH.
A special thank you to the unsung heroes who are working at the NIH Clinical Center in a shifting and uncertain environment. This especially includes the staff of Materials Management and Environmental Services Department who are tasked with ensuring personal protective equipment (PPE) is available at a time of national shortages, especially since that flooding last summer wiped out stocks of equipment the hospital had on hand and they had to build this inventory from scratch.
At the end of May, the NIH Clinical Center began to phase-in several hundred employees back to work physically within the hospital since the coronavirus disease 2019 (COVID-19) pandemic swept across the nation mid-March. The hospital also began to slowly increase the patient census from roughly 50 to around 100 inpatients and outpatient clinic visits from roughly 50 a day to 150 a day.
"We are being asked to lead the reopening of the NIH campus and it's a responsibility that I think we should be proud of but it's a responsibility that means we have to be really cautious and careful how we do that," said Dr. Jim Gilman, CEO of the Clinical Center, during a Town Hall May 6 (NIH Staff Only).
"This is not a return to business as usual. There is nothing like our usual," Gilman said. "Since March 11, Clinical Center efforts were limited to the most urgent patients. I think we are mature enough in our infection control measures and our understanding of what it takes to work in this pandemic to begin to increase our patient census."
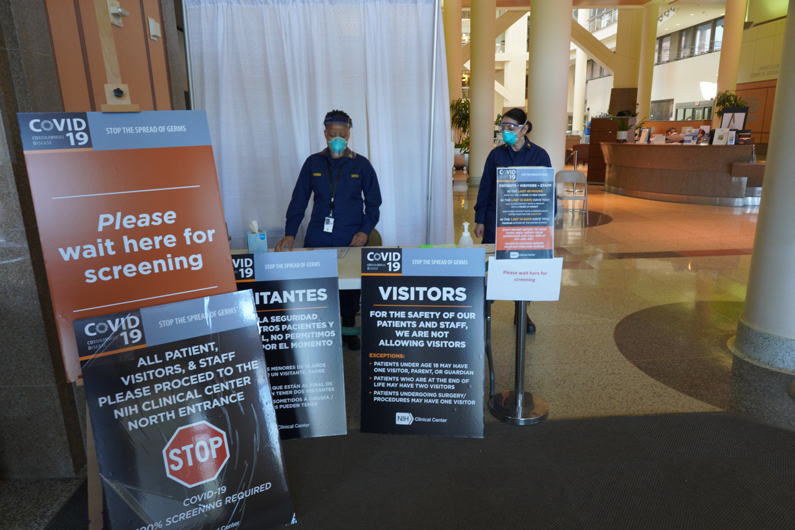
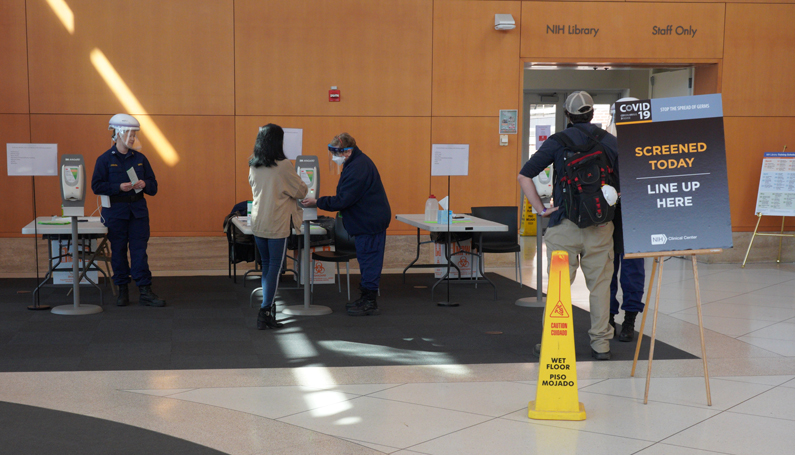
Anyone entering Building 10 – including patients, visitors, construction workers, researchers and staff – are screened at the North Lobby, Ambulance Entrance or P1 Parking Entrance Lobby by the U.S. Public Health Service Commissioned Corps Nursing Officers and are instructed to wear surgical masks. On May 20, the hospital hit a milestone of screening its 100,000th person entering Building 10.
"The safety of our patients and staff cannot be jeopardized," Gilman added during the Town Hall. "We can never forget we're doing this in the middle of a pandemic."
Existing infection control measures also include restriction of visitors, staff working in segregated teams, social distancing (including in clinics and departmental waiting rooms), no large group meetings and keeping Building 10 cafeterias closed. The atrium coffee shop remains open with expanded offerings.
Current inpatients, and any who may be enrolling in a trial over the coming weeks, can only have visitors who agree to room-in, be tested for COVID, and stay with the patient. Outpatients who require visual or ambulatory assistance will be allowed to have a family member or escort. When a patient is admitted to hospital, they will undergo syndromic screening upon admissions.
As the patient census increased, prospective surveillance testing of all NIH employees in the building with direct patient care began May 21. While voluntary, employees are strongly encouraged to schedule themselves to participate in the Clinical Center's weekly surveillance testing.
While the initial phase-in of staff physically present in Building 10 began – the vast majority of NIH campus, all those who are telework-eligible employees, still remain offsite. On May 15, Julie Berko, the director of the NIH Office of Human Resources, presented a framework for NIH employees for return to physical workspaces (NIH Staff Only). She announced that NIH is shifting to a maximum telework "until further notice" – an extension from the original timetable of "through May 31" announced by Dr. Francis Collins, Director of NIH, on April 24.
Hospital Epidemiology Service resources, including details about testing patients and staff (NIH Staff Only)
NIH Guidance for Staff on Coronavirus (NIH Staff Only)
NIH Town Hall May 21 (NIH Staff Only)
Sailing Close to the Breeze: Hospital Epidemiology in the COVID-19 Pandemic: May 20 lecture by Dr. Tara Palmore, CC Hospital Epidemiologist (HHS Only)
COVID-19 Diagnostics: The Challenge of Rapid, High-Volume Detection of SARS-CoV-2: April 28 lecture by Dr. Karen Frank, CC Chief of the Department of Laboratory Medicine
Preparing For COVID-19 Patients
Through its approximately 1,600 clinical research trials, the NIH Clinical Center provides care for many severely immunocompromised patients. When reports of a previously unknown, highly contagious virus emerged early in 2020, the hospital's leadership understood the impact the coronavirus could have on this population.
In early February, the Diamond Princess cruise ship with 3,700 passengers aboard, identified COVID-19 cases. The ship was put into quarantine in Japan and discussions began about repatriating the over 400 Americans on board. As a globally-recognized medical research center, the Clinical Center quickly and quietly prepared for patients.
The hospital's leadership activated a 24/7 emergency operations center staffed by a multi-disciplinary team of medical experts to address the wide range of constantly changing scenarios.
As the pandemic evolved, the team's planning quickly escalated from a daily meeting to as many as five meetings a day. Building on the successful treatment of patients with Ebola virus disease in 2014 and 2015, staff incorporated new strategies to keep research hospital staff and patients safe while addressing this public health crisis.
In preparation, the hospital activated its Special Clinical Studies Unit (SCSU) – an inpatient unit designed with state-of-the-art infrastructure for isolation and infection control – as well as an inpatient unit with respiratory isolation and staffed by infectious diseases and critical care specialists.
The Clinical Center conducted a practice run with the SCSU, the NIH Division of Fire and Rescue Services and the NIH Police to better prepare staff to receive and transfer COVID-19 patients among healthcare facilities.
The hospital also shares information, expertise, resources and patient care with the Bethesda Hospital Emergency Preparedness Partnership. The partnership includes Walter Reed National Military Medical Center, Suburban Hospital and the National Library of Medicine.
The hospital implemented a COVID-19 testing program to help protect patients and staff and provide laboratory services for other hospitals in the National Capital Region.
While the passengers with COVID-19 from the Diamond Princess were eventually quarantined and treated at other locations, the SCSU and inpatient units are now being used for the treatment of staff and patients who test positive for COVID-19.
"The nursing staff feels very fortunate to be working here at the Clinical Center. We trust the experts who are advising us and we have sufficient stock of personal protective equipment (PPE) to deal with the patients," said Cecelia Henry, Service Educator in Oncology and Critical Care Service. "We appreciate the forethought and high degree of accountability that has gone into this effort."
During the month of April, about twelve patients with COVID-19 were treated in the SCSU. Most were enrolled in a treatment trial of remdesivir, an antiviral medication used as a treatment for Ebola virus disease and Marburg virus infections and found to show antiviral activity for coronaviruses (including MERS and SARS viruses).
- Debbie Accame and Lester Davis
Stopping COVID-19 at the Door
Protecting patients and staff from contracting and spreading the COVID-19 virus is a priority for the NIH Clinical Center. This is being accomplished in three ways.
First, to limit the possibility of unintentional infection, hospital staff are not to report to work if they have COVID-19 symptoms or a high risk of exposure to the virus.
(Updated 7/8/2020)
These symptoms include:
- New fever (37.5°C/99.5°F)
- New cough
- New loss of taste or smell
- Sore throat
- Muscle or body aches
- Headache
- Shortness of breath
- Congestion or runny nose
- Diarrhea
- Nausea or vomiting
Staff with these symptoms must immediately go home, notify their supervisor and call the NIH's health service, the Occupational Medical Service (OMS) response center at 301-496-4411.
OMS is a part of the Division of Occupational Health and Safety and offers medical assistance to NIH employees (federal, contractor, trainee and others). The response center is open to answer questions and conduct health screenings for employees who are sick and/or have a reasonable concern that they have been exposed to the COVID-19 in the past 14 days.
Secondly, staff and visitors are being screened at Building 10 entrances by the U.S. Public Health Service Commissioned Corps Nursing Officers.
"Our goal is to protect patients, family members, visitors and staff. As public health officers, we provide education about the COVID-19 virus, what to do if symptoms develop and who to contact," said Capt. Ann Marie Matlock, with the U.S. Public Health Service, Service Chief of the Medical Surgical Specialties at the Clinical Center. "We talk to patients, family members and staff about their concern and fears to help lessen their anxiety and answer any questions they may have. We are working on the front lines to make this happen."
Finally, as of April 2, everyone entering Building 10 – including patients, visitors, construction workers, researchers and staff – are instructed to wear surgical masks.
As of May 19, there are 162 known cases of NIH employees diagnosed with COVID-19. All diagnosed staff have gone through contact tracing and comprehensive cleaning of their workspaces.
"From a Clinical Center perspective, we trained for COVID-19 for two years, not two months, two years," said Dr. James Gilman, CEO of the Clinical Center at the hospital's virtual Town Hall on April 8. "Because on an almost weekly basis, we have emphasized how important it was to keep our patients safe by not spreading infections."
The OMS response center is open from 9 am – 4:30 pm (weekdays), 10 am – 2 pm (Saturdays), and from 9 am – 4:30 pm (Sundays).
- Lester Davis and Mickey Hanlon
At NIH: Empty Offices, Quiet Labs
The announcement was unprecedented in the history of NIH. The World Health Organization publicly declared a pandemic on March 11. On March 13, the message came from NIH Director Francis S. Collins.
"I have made the decision that effective Monday, March 16, all telework-eligible employees across the NIH should begin teleworking to the extent possible" through April 3. Collins later added that "Given the evidence that the COVID-19 pandemic is unlikely to come under control soon" the telework mandate would be extended to at least May 1. On April 24, telework was further pushed to May 31. Then on May 15, it was pushed "until further notice."
NIH instructed all supervisors to provide flexibility to staff, as many of them were juggling their work responsibilities as well as managing care for children or elders who had their previous schooling and care arrangements adjusted on short notice.
While the initial guidelines applied to administrative and staff working on research programs outside of the NIH campus, on March 23 the guidelines expanded to include the NIH Intramural (onsite) Research Program. NIH labs moved to minimize the physical presence of staff in NIH laboratories, to support only mission-critical functions.
There are over 1,000 research laboratories at the NIH campus, with dozens of them in the Clinical Center. The Intramural Research Program developed guidelines to limit laboratory operations, in order to maximize social distancing. This effort attempted to balance safety of personnel with carrying out mission critical functions.
Labs that utilize animals, such as mice and fruit flies, or certain mechanical equipment, such as powerful magnets for NMR or liquid nitrogen freezers, are required to limit their presence in the lab to only one staff person at a time.
The guidelines state that in most cases, laboratory personnel should not be in the labs at all. This skeleton crew approach focuses on maintaining certain critical functions and to avoiding the loss of resources.
"A minimal maintenance effort means no two people in the same place at the same time," noted Dr. Michael M. Gottesman, deputy director for Intramural Research at the NIH. "For example, my lab has someone who comes in for an hour a day to check on freezers, packages, plumbing and such. This is one person per 80 total staff. Should any lab have more? No, not unless there are mission critical activities going on in the lab. And even then, no one should be at risk."
There are some exceptions: care of patients in non-elective NIH clinical protocols; direct research on COVID-19; urgent public health research recommended by a leading research director and approved by a research subcommittee of the NIH COVID-19 Response Team; work involving significant research investments that could be lost if not continued (also to be reviewed by the Response Team subcommittee), and the protection of life, property and resources, including the care of research animals.
Dr. Leslie Biesecker, chief of the Medical Genomics and Metabolic Genetics Branch at the National Human Genome Research Institute, said he was totally committed to Dr. Collins' mandate to work remotely. His lab has been working with NIAID and NCI to study the host genetics of COVID -19 disease, to determine potential factors that may determine who is more vulnerable to the virus.
"We can do a lot remotely," said Biesecker. "If we work at it, it's surprising what we can accomplish."
As the social distancing measures continue, their impact on the hospital has been clear. Traffic in the Clinical Center has been reduced by 85-90%.
- Debbie Accame and Donovan Kuehn

